Understanding the Types of Health Insurance Plans – Health insurance is a crucial component of healthcare in the United States and many other countries, providing individuals with access to necessary medical services while mitigating the financial burden of healthcare costs.
With a variety of plans available, understanding the differences between these options can empower consumers to make informed decisions. This article explores the major types of health insurance plans, their benefits, drawbacks, and contexts in which they might be most appropriate.
Health Maintenance Organization (HMO)

Overview
Health Maintenance Organizations (HMOs) are a common type of managed care plan that offers a network of doctors and hospitals. To receive full benefits, members must choose a primary care physician (PCP) and obtain referrals to see specialists.
Benefits
- Cost-Effective: HMOs often have lower premiums and out-of-pocket costs compared to other plans.
- Coordinated Care: The requirement to have a primary care physician ensures that all aspects of a member’s healthcare are coordinated.
- Preventive Services: Many HMOs emphasize preventive care and may offer it at no additional cost.
Drawbacks
- Limited Provider Network: Members are typically restricted to a specific network of healthcare providers, which can be limiting.
- Referral Requirement: The necessity for referrals can be cumbersome for patients needing to see specialists.
- Less Flexibility: If members seek care outside the network without a referral, they often face significantly higher costs.
Ideal for
Individuals who prefer lower costs and do not mind using a smaller network of healthcare providers may find HMOs advantageous.
Preferred Provider Organization (PPO)
Overview
Preferred Provider Organizations (PPOs) offer more flexibility in choosing healthcare providers. Members can see any doctor or specialist without a referral, although costs will be lower when using in-network providers.
Benefits
- Flexibility: Members are not required to select a primary care physician and can see specialists directly.
- Broader Network: PPOs usually have a larger network of providers compared to HMOs, allowing for more options.
- Out-of-Network Coverage: Members can receive care from out-of-network providers, albeit at a higher cost.
Drawbacks
- Higher Costs: Premiums and out-of-pocket expenses are generally higher than those of HMOs.
- Complex Billing: The flexibility can lead to confusion regarding billing and claims, especially when using out-of-network services.
- Cost-Sharing: Members may face high deductibles and copayments, especially when not using in-network providers.
Ideal for
Individuals who prioritize flexibility and choice in their healthcare providers may prefer PPO plans.
Exclusive Provider Organization (EPO)
Overview
Exclusive Provider Organizations (EPOs) are similar to PPOs in that they do not require referrals to see specialists but differ in that they do not provide any out-of-network coverage except in emergencies.
Benefits
- No Referral Requirement: Members can directly access specialists without needing a referral.
- Lower Premiums: EPOs often come with lower premiums compared to PPOs due to their limited network.
- Cost Savings: Because they manage costs through their exclusive networks, they can offer savings on out-of-pocket expenses.
Drawbacks
- Limited Provider Choices: Members must use the network of providers to receive any benefits, leading to potential limitations on care.
- No Out-of-Network Benefits: Unlike PPOs, EPOs do not cover services outside their network, which can pose a risk if a member requires specialized care not available in-network.
- Emergency Situations: In emergencies, members may be forced to seek care outside of their network, leading to confusion about coverage.
Ideal for
Individuals who want lower premiums but still value the ability to see specialists without referrals may find EPOs suitable.
Point of Service (POS)
Overview
Point of Service (POS) plans combine features of HMOs and PPOs. Members have the option to choose between in-network and out-of-network providers, but like HMOs, they usually need a primary care physician and referrals for specialists.
Benefits
- Combined Features: POS plans offer the ability to use both in-network and out-of-network providers, providing flexibility.
- Lower Costs for In-Network Care: Members can enjoy lower costs when utilizing in-network services.
- Coordinated Care: The requirement for a primary care physician encourages coordinated care.
Drawbacks
- Higher Costs for Out-of-Network Care: Members face higher out-of-pocket expenses when seeking care outside the network.
- Referral Requirement: Like HMOs, members must obtain referrals to see specialists, which can be inconvenient.
- Complexity: Understanding the balance between in-network and out-of-network services can be confusing for members.
Ideal for
Individuals who want a balance between flexibility and cost-effectiveness may find POS plans appealing.
High-Deductible Health Plans (HDHP)
Overview
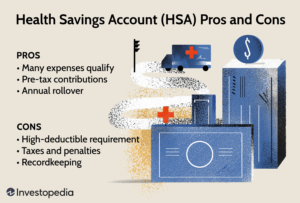
High-Deductible Health Plans (HDHP) have higher deductibles than traditional health plans but often come with lower premiums. They are commonly paired with Health Savings Accounts (HSAs) that allow members to save for medical expenses tax-free.
Benefits
- Lower Premiums: HDHPs generally have lower monthly premiums compared to other plans.
- HSAs: The ability to contribute to HSAs provides tax advantages for saving for healthcare costs.
- Preventive Coverage: Many HDHPs cover preventive services at no cost before the deductible is met.
Drawbacks
- High Out-of-Pocket Costs: Members may face significant costs before the deductible is met, which can be a barrier to care.
- Financial Risk: The high deductible can lead to financial strain if unexpected medical expenses arise.
- Complexity: Understanding the intricacies of HDHPs and HSAs can be challenging for some consumers.
Ideal for
Individuals who are generally healthy and do not expect significant medical expenses may find HDHPs appealing due to their lower premiums.
Medicare and Medicaid
Overview
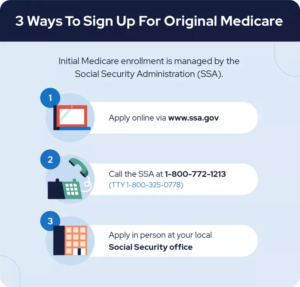
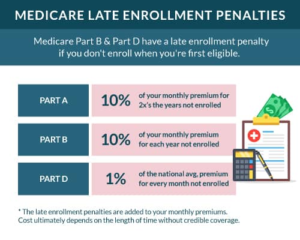
Medicare and Medicaid are government-sponsored health insurance programs designed for specific populations. Medicare primarily serves seniors and certain disabled individuals, while Medicaid provides coverage for low-income individuals and families.
Benefits
- Comprehensive Coverage: Both programs provide a wide range of services, including hospitalization, outpatient care, and preventive services.
- Cost-Effectiveness: For eligible individuals, these programs often cover a large portion of healthcare costs, significantly reducing out-of-pocket expenses.
- Accessibility: These programs enhance access to healthcare for vulnerable populations.
Drawbacks
- Eligibility Requirements: Navigating the eligibility criteria for these programs can be complex.
- Limited Provider Networks: Some Medicaid plans may have limited provider networks, which can reduce access to care.
- Potential for Underfunding: Both programs can face funding challenges, which may impact the availability and quality of services.
Ideal for
Seniors, low-income individuals, and families may find Medicare and Medicaid essential for accessing affordable healthcare.
Conclusion
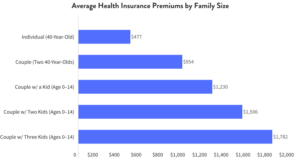
Choosing the right health insurance plan is a critical decision that can significantly impact an individual’s or family’s access to healthcare services and financial well-being. By understanding the various types of health insurance plans—HMO, PPO, EPO, POS, HDHP, Medicare, and Medicaid—consumers can better assess their needs and financial situations.
As the healthcare landscape continues to evolve, it is essential for individuals to stay informed about their options, consider their healthcare needs, and analyze the benefits and drawbacks of each type of plan. Ultimately, the right choice will depend on personal circumstances, preferences, and financial capabilities.